Autism Management:
General principles of management: Autism Spectrum Condition (ASC) can present substantial barriers to normal daily functioning and the approach to its management is a combination of symptom modification together with the removal of these barriers wherever possible.
Pharmacological Interventions:
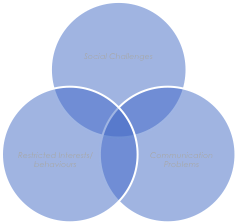
No medication has any direct effect on the triad of impairment (social challenges, restricted interests/behaviours and communication problems) in ASC and the place of medication is therefore mainly in alleviating associated conditions and problems. The risks should always be looked at in balance with the small potential benefits.
Additional cautions are advised when using any medications in autism because of the increased likelihood of unpredictable effects in this group of patients.
Antidepressants in ASC for Anxiety and Depression
SSRI (Selective Serotonin Reuptake Inhibitor): are sometimes an effective treatment for severe Anxiety and depression in Autism.
SSRI treatment of Anxiety and Depression commonly used in children are Fluoxetine, Sertraline, fluvoxamine and escitalopram.
SSRI treatment of Anxiety and Depression in adults are Fluoxetine, Escitalopram, fluvoxamine, Paroxetine and Sertraline.
Catatonia and ASC
There are various theories about the relationship between catatonia in autistic children and adults. Catatonia can be defined as a group of symptoms that usually involve difficulties in movement and behaviour (Diagnostic and Statistical Manual of Mental Disorders-IV DSM-IV: American Psychiatric Association, 2013). The Overlap in the clinical pictures of catatonia, autism and parkinsonism raises the question as to whether they are all part of a continuously distributed array of disorders of movement and volition related to the extrapyramidal system. Some individuals show a tendency to passivity in social interactions before the onset of catatonia, suggesting a difficulty in initiating motor activity as a possible neuropathology in the three conditions, although autism is also a social and cognitive condition (Wing & Shah, 2000).
Treatment of catatonia is lorazepam
Self-injurious behaviour in ASC:
Self-injurious behaviour (SIB) includes slapping, punching, banging and biting. In practice, the most common causes of self-injury are pain and low mood.
The presence of SIB points to particular genetic syndromes that are more common in patients with a lower than average IQ. The majority of SIBs can be managed using behavioural approaches and treating anxiety; however, when SIBs are more serious and these strategies prove ineffective, pharmacotherapy may be an option, although the evidence base is lacking.
Prescribing standards
When discussing potentially prescribing medication off-licence, it is important to:
• Explain to the patient and carers that the medication is not licenced for the intended use
• Explain the intended benefits and possible side-effects
• Ensure the patient/carer is in complete agreement before prescribing
• Provide them with information leaflets, if available.
Documentation
The discussion must be clearly documented in the patient's notes. The Royal College of Psychiatrists provides four standards that should be followed in its FR/ID/09 practice guidelines (RCPsych, 2016).
• Pharmacological approaches should not routinely be used to treat the core features of autism and should never be used in isolation.
• The common associated symptoms of irritability, stereotypies and compulsions, hyperactivity and ADHD, and sleep difficulties can potentially be treated pharmacologically. The ABC is a caregiver-scored report of behaviour commonly used.
• The stereotypies seen in ASD differ from those seen in OCD as they often have a sensory basis and can in fact calm the person down. The evidence base for selective serotonin reuptake inhibitors (SSRIs) is variable.
• When prescribing off-licence, it is important to follow the four standards set out in the Royal College of Psychiatrists' FR/ID/09 practice guidelines (RCPsych, 2016).
1) American Psychiatric Association. (2013). American Psychiatric Association, 2013. Diagnostic and statistical manual of mental disorders (5th ed.). In the American Journal of Psychiatry. https://doi.org/10.1176/appi.books.9780890425596.744053
2) Coghill, D., Bonnar, S., Duke, S., Graham, J., Seth, S., Coghill, D., Bonnar, S., Duke, S., Graham, J., & Seth, S. (2011). Classification of disorders. In OSH Child and Adolescent Psychiatry. https://doi.org/10.1093/med/9780199234998.003.0002
3) Goodman, R., & Scott, S. (2012). Child and Adolescent Psychiatry: Third Edition. In Child and Adolescent Psychiatry: Third Edition. https://doi.org/10.1002/9781118340899
4) National Institute for Health and Care Excellence. (2016). Autism spectrum disorder in adults: diagnosis and management. NICE Guidance and Guidelines.
5) Wing, L., & Shah, A. (2000). Catatonia in autistic spectrum disorders. British Journal of Psychiatry. https://doi.org/10.1192/bjp.176.4.357
6) World Health Organization. (1993). The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. In The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research.
You might find these interesting too!
Robert shares his and his wife’s experience and advice in caring for a child with autism and an eating disorder.
A neurodiversity-informed guide for patients with an eating disorder, with a focus on autism and ADHD. This resource offers practical information and strategies grounded in lived experience and clinical expertise.
This lived experience piece explores how receiving an autism diagnosis shaped two individuals’ journeys through eating disorder recovery. They reflect on the challenges they faced in treatment before understanding their neurodivergence, how the diagnosis reframed their experiences, and how recovery strategies became more effective when adapted to their sensory and cognitive needs. Their stories highlight the importance of autism-informed approaches in eating disorder care.